Author: Devin Bland, DPM, FACFAS, DABPM, Prestige Medical Care, Phoenix, AZ.
INTRODUCTION
Flatfoot (also referred as pes planus) describes a reduction or absence of the foot medial longitudinal arch (MLA), with or without additional foot and ankle deformities. Flatfoot is relatively common in childhood, with flexible flatfoot being its most common form, affecting up to 14% of children1. Rigid flatfoot, known as peroneal spastic flatfoot, is present in only about 1% of flatfeet in children and characterized by the absence of the arch even in the absence of weight bearing2. It is usually diagnosed between the ages of 8-16, most frequently followed by pain2,3. Rigid flatfoot can be the result of a tarsal coalition (TC), an infrequent disorder demonstrating fusion (bridging) of two or more tarsal bones. It exists at birth but usually does not become symptomatic until teenage years or afterwards. Tarsal coalition often results in decreased mobility, pain and deformity, leading to a rigid planovalgus foot2,4. Calcaneonavicular (CN) coalition, the most frequent form (53%), may induce pain and restricted subtalar and ankle range of motion (ROM). Unfortunately, CN coalitions usually respond poorly to conservative treatment. In these cases, it is established that surgical resection is mandatory5. Since those are commonly pediatric procedures, high attention is dedicated to maintaining the integrity of the child’s growth plates.
CASE PRESENTATION
A 10-year-old male patient, weighing of 130 lbs. The patient was diagnosed with spastic pes planus, as well as posterior tibial tendinitis of the right foot. The patient complained of difficulty in walking and reported extreme right lower extremity pain, manifested especially during ambulation and physical activity. MRI has shown fibrotic coalition of the calcaneonavicular bones, which was considered a congenital deformity. Also present, focal bone marrow edema along the proximal aspect of the cuboid, which may be representative of stress reaction or osseous contusion. The subtalar and Tibio-talar joints were normal, with no osteochondral lesions and all ligaments and tendons were intact. As all conservative treatment options failed, including bracing, inserts, shoe and activity modification as well as physical therapy, the family opted for an elective surgical repair.
WHY OSSIOfiber® IS AN IDEAL CHOICE FOR THIS PATIENT?
The patient is a 10-year-old boy, therefore sparing his joints and avoiding permanent hardware in his feet has higher importance compared to an adult patient.
It was decided that OSSIOfiber® would be the ideal choice of treatment for this patient, providing stable fixation and stabilization for the healing period with no hardware remaining long term.

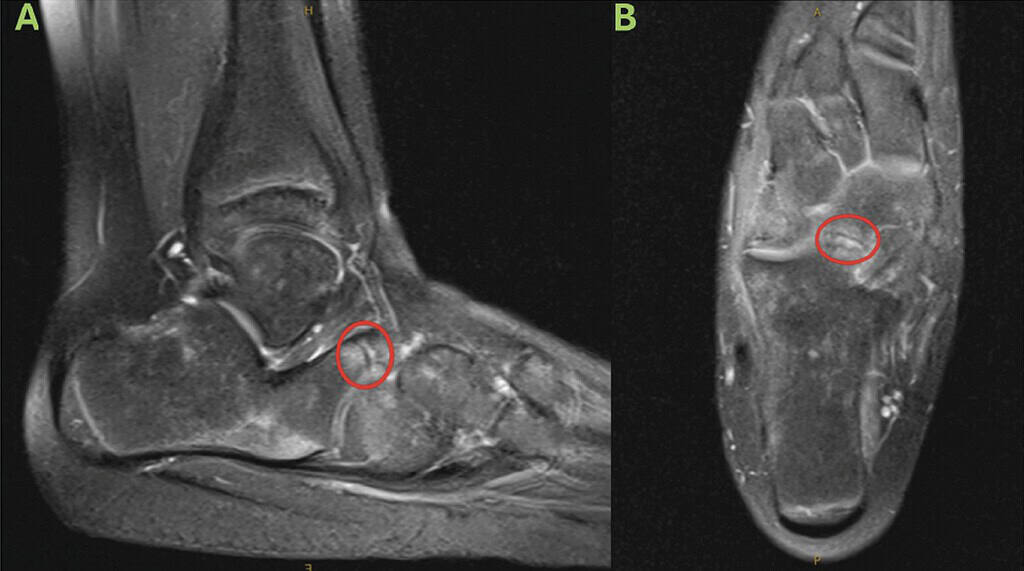
coalition (red circles), with diffuse patchy marrow edema throughout the imaged osseous structures. Main focal marrow edema is present along the proximal aspect of the cuboid.
Surgical Plan
Calcaneal osteotomy, midfoot osteotomy and removal of calcaneonavicular coalition.
The following OSSIOfiber® fixation implants were used:
- OSSIOfiber® Threaded Trimmable Fixation Nail (TTFN) 4.5x70mm x 2 units
- OSSIOfiber® Compression Staple 11x10mm x 1 unit
Accompanying Devices:
- Demineralized Bone Matrix (DBM) Allograft
- Tricortical Wedge Allograft (MTF Biologics)
Surgical Technique
The patient was placed in a supine position.
- Calcaneal osteotomy: Bicortical osteotomy was done achieving approximately 1cm of translocation of the capital fragment. Meticulous care was taken to avoid harm to the growth plates. Two OSSIOfiber® 4.5mm Threaded Trimmable Fixation Nails were cut to 44mm length following over-the-wire depth measurement, and placed far and clear away from the growth plate, creating a strong stabilization.
- Coalition removal: Focusing on the dorsal part of patient foot, the coalition present between the calcaneus and the navicular bones was managed under direct fluoroscopy. A linear incision was created, and the origin of the coalition was then resected and cauterized. Following coalition resection, the subtalar joint range of motion showed great improvement and was deemed anatomic.
- Posterior Tibial Tendon Debridement: Meticulous care was taken to identify the Posterior Tibial Tendon. There was a moderate amount of synovitis present. Careful debridement was carried out with repair as needed.
- Cotton wedge midfoot osteotomy: An opening wedge osteotomy of the medial cuneiform was done (i.e. Cotton) and packed with the Tricortical Allograft and 1cc of DBM Allograft. Then, an OSSIOfiber® 11x10mm Small Compression Staple was placed across the osteotomy for fixation.
- Gastrocnemius recession: Following the above procedures a weightbearing simulation was carried out. Although a good correction was achieved, identifying isolated gastrocnemius contracture by the Silfverskiold test dictated a gastrocnemius recession which was performed from a medial approach in standard technique with no complications noted.
- Patient was then placed in a modified bulky Jones splint at approximately 90 degrees. A brisk capillary refill time was noted and a prompt hyperemic response. The patient remained in the splint until the first post-operative visit, 4 weeks post-op.
Post-Operative Protocol
A well-padded Bulky Jones splint was applied until the first post operative visit, then the patient was transitioned to a short leg cast.
- Non-weight bearing: Four weeks post operative from the date of surgery.
- Partial weight bearing: In a CAM boot, starting at four weeks for the next two weeks.
- Full weight bearing: At 6 weeks post-op in a comfort shoe. start physical therapy.
Patient Follow-up:
The patient showed a quick and complication free post-operative presentation. The incision showed progressive healing through each visit of the four non-weight bearing weeks and the foot and the ankle were free of edema. At four weeks, the patient transitioned to protected weight bearing in a CAM boot. At six weeks, the patient transitioned to normal athletic shoes and started working on his dorsiflexion, eversion, inversion and gait pattern with physical therapy. From 6 weeks to 14 weeks the patient was in normal athletic shoes, walking with no restrictions and attending PT to learn how to ambulate with his new corrected foot pattern. By 14 weeks the patient demonstrated complete healing as shown on final postoperative x-rays.


The growth plates are still noted as open.
Summary
OSSIOfiber® is a revolutionary thorough, with this case illustrating its versatility. Pediatric patients pose a unique complexity to revision surgery. Traditional metallic implants frequently require removal as the young patient grows and the osseous anatomy changes in size. OSSIOfiber® allows complex pediatric corrections with the ability to have the implants incorporate with the ever-changing osseous anatomy, eliminating the necessity of hardware removal.
References
- Turner, C., Gardiner, M .. , Midgley, A. & Stefanis, A. A guide to the management of paediatric pes planus. Aust. J. Gen. Pract. 49, 245-249 (2020).
- Vukasinovic, Z .. et al. Flatfoot in children. Acta Chir. lugosl. 58, 103-106 (2011).
- Jayakumar, S. & COWELL, H . . Rigid flatfoot. Clin. Orthop. Relat. Res. 122, 77-84 (1977).
- Efstathopoulos, N., Nikolaou, V., Lazarettos, J., Triantopoulou, C. & Plessas, S. Calcaneonavicular coalition. Eur. J. Orthop. Surg. Traumatol. 16, 70-74 (2006).
- Knl:lrr, J. et al. Arthroscopic treatment of calcaneonavicular coalition in children. Orthop. Traumatol. Surg. Res. 97, 565-568 (2011).
