Author: Jue Cao, MD, FAAOS., HCA HealthONE Rocky Mountain Children’s Hospital, Denver, CO
INTRODUCTION
Carpal coalitions is a rare anatomical abnormality, characterized by the union of two or more carpal bones and caused by a defect in the separation and cavitation process during embryonic development. As most patients with congenital carpal coalitions are asymptomatic and found incidentally, the incidence of carpal coalitions varies from 0.1% in white Americans to up to 9% in South African Bantu. It is twice as common in females as in males.1-3 Two primary forms of carpal coalition exist: Osseous (synostosis) and non-osseous. In an osseous coalition, referred to as a complete coalition, the carpals are united as a single osseous block. Whereas, in a non-osseous coalition, referred to as an incomplete coalition, the affected carpals are united either by cartilage (synchondrosis), fibrous tissue (syndesmosis), or both.4
Although largely asymptomatic, symptoms may manifest secondary to biomechanical stress at the site of fusion. In patients with symptomatic incomplete coalitions, lunate and triquetrum fusion provides acceptable results with little wrist dysfunction.
CASE HISTORY
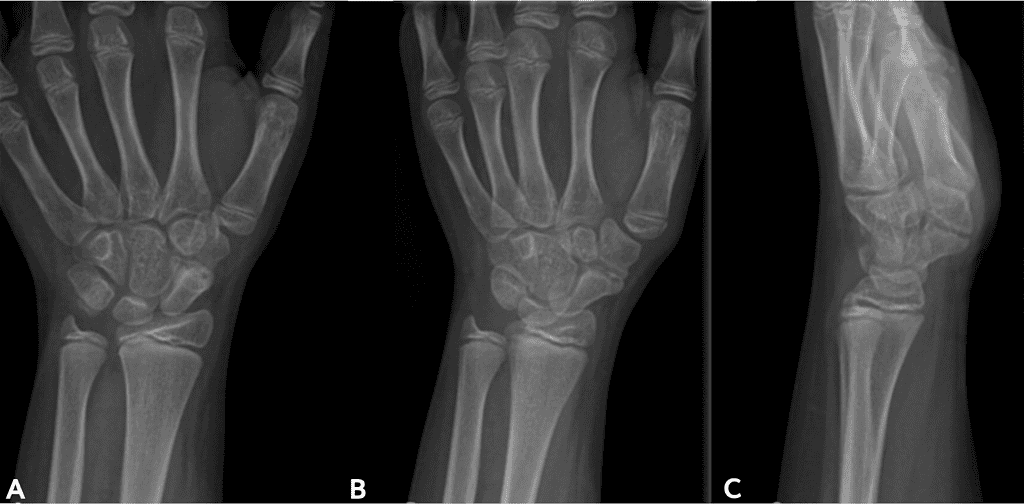
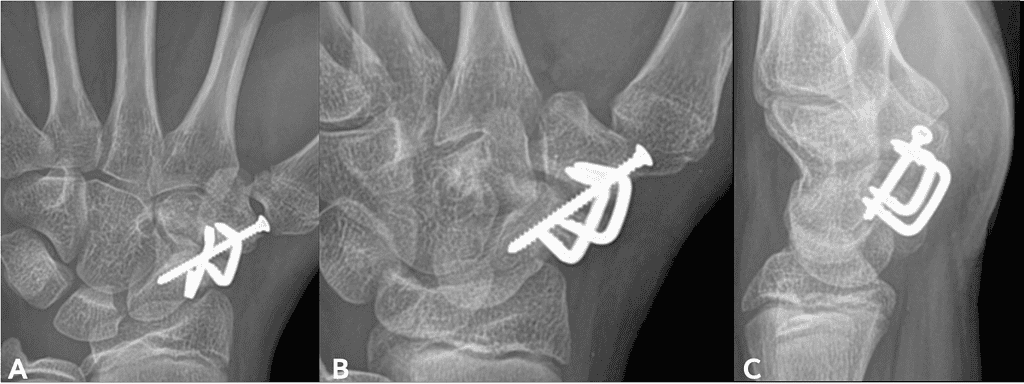
The patient is an 11-year-old right-hand dominant female with a symptomatic scaphoid-trapezial synchondrosis, initially presenting with chronic left wrist and hand pain without a history of trauma. She previously underwent attempted surgical fixation and fusion of the synchondrosis with 2 K-wires in November 2022, which failed to achieve union. A subsequent revision fusion was performed in December 2023 using two titanium BME™ staples and a stainless-steel screw; however, despite prolonged immobilization, vitamin D optimization, and bone stimulation therapy, the patient continued to have persistent pain and radiographic evidence of nonunion at the scaphoid-trapezial joint.
CASE PRESENTATION
At her evaluation on February 2025, 14 months following her second procedure, the patient exhibited persistent pain localized to the scaphoid-trapezial joint. She reported pain with palpation over the joint and with most wrist-dependent activities, including participation in volleyball. Radiographs demonstrated a persistent nonunion at the scaphoid-trapezial fusion site, along with loosening of the stainless-steel hardware.
Given her ongoing symptoms, functional limitations, and failure of prior fusion attempts, the decision was made to proceed with revision scaphoid-trapezial fusion, including removal of loose metal hardware, utilizing OSSIOfiber® implants and a vascularized distal radius bone graft.
The goal of this procedure is to achieve bony union, restore wrist stability, and relieve pain.
WHY OSSIOfiber® IS AN IDEAL CHOICE FOR THIS PATIENT?
There were two primary reasons OSSIOfiber® was selected for this case. Most importantly, OSSIOfiber®’s osseous integration properties provide stable fixation enabling bone formation and enhancing the likelihood of achieving fusion across the joint. Additionally, because OSSIOfiber® implants are biointegrative and fully resorbable, they do not require removal. This significantly reduces the risk of future hardware-related symptoms, particularly important in a pediatric patient. By providing both mechanical stability and biointegrative augmation, the biointegrative OSSIOfiber® implants offer the added benefit of acting as a scaffold to support bone healing in this revision fusion construct.
Figures 1-3 below descript the patient initial medical condition and subsequent surgical procedures prior to use of OSSIOfiber® implants
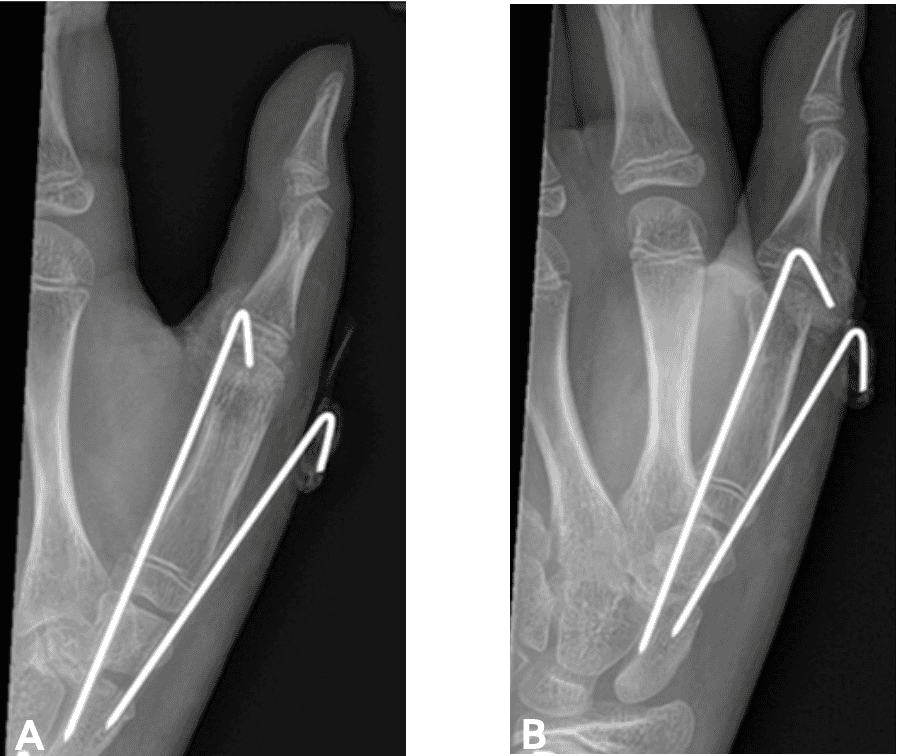
Oblique thumb view [A] and Lateral thumb view [B]
Surgical Plan
Left scaphoid-trapezial revision fusion with vascularized bone graft from the distal radius, Left wrist hardware removal.
Preoperatively, the diameter of the scaphoid was assessed to determine the appropriate implant size. A 3.5 mm OSSIOfiber® headless Compression Screw was selected for optimal compression across the scaphoid-trapezial joint. In addition, the prior BME™ staples were planned to be replaced with OSSIOfiber® compression staples.
The following OSSIOfiber® fixation implants were used:
- OSSIOfiber® Compression Screw (CS) 3.5x22mm
- OSSIOfiber® Small Compression Staple 11x10mm x 2 units
Surgical Technique
A volar approach to the scaphoid was utilized, with proximal extension to the distal radius to facilitate a physeal-sparing harvest of a vascularized distal radius bone graft, using the technique previously described by Mathoulin.5
- First Approach: A longitudinal incision was made along the patient’s prior thenar eminence incision, extending approximately 6 cm along the Flexor Carpi Radialis (FCR) tendon. Full-thickness skin flaps were elevated. A branch of the radial sensory nerve was identified, carefully released from scar tissue, and protected throughout the procedure.
The previous incision between the thenar muscles and the volar joint capsule of the scaphoid-trapezial joint was deepened down to the joint. Two loose titanium staples and one unstable metal screw were removed. The scaphoid-trapezial joint, which had failed to fuse, was identified. Fibrinous tissue was debrided using a Freer elevator and rongeur to prepare the fusion site. - Graft Harvest: Attention was directed to the distal radius. Blunt dissection was carried into the potential space of Parona. The distal margin of the pronator quadratus (PQ) was identified, along with a traversing vessel from the radial to the ulnar side. The distal PQ fascia was incised horizontally, and the PQ was retracted proximally to expose the vessel.
Under fluoroscopic guidance, a 1 x 1 cm periosteal window was created along the ulnar border, carefully avoiding the distal radial physis and distal radioulnar joint. A tricortical vascularized bone graft was harvested based on the pedicle vessel. The periosteum was sutured back to the cortical bone to prevent displacement.
Due to the small size of the tricortical graft relative to the defect, an additional cancellous bone graft was harvested from the distal radial metaphysis using a curette. The cancellous graft was then packed into the prepared scaphoid-trapezial joint. - Graft Placement and Fixation: The vascularized tricortical graft was positioned along the volar surface of the scaphoid-trapezial joint. The tourniquet was temporarily released to confirm excellent bleeding from the graft, confirming vascular integrity, and then re-elevated.
An antegrade K-wire was placed from the dorsal scaphoid into the trapezium under fluoroscopic guidance, ensuring correct placement on orthogonal views.
A 1 cm longitudinal incision was made in the skin, at the entry of the k-wire dorsally with blunt dissection with a hemostat down to the proximal scaphoid pole. The extensor tendons were protected before drilling over the K-wire for the headless compression screw. A headless 3.5mm OSSIOfiber® compression screw was placed between the scaphoid and trapezium to achieve initial fixation. The K-wire was then removed.
Given concern for graft stability, a second fixation was added from the volar surface. A 11x10mm compression staple was placed to compress the vascularized graft without compromising the vascular pedicle. Drill holes were prepared carefully, and the implant was introduced without interfering with the headless compression screw.
The construct was stable without tension or kinking on the vascular pedicle. Wrist range of motion showed full mobility without motion at the scaphoid-trapezial joint. - Intraoperative Imaging: Final fluoroscopic imaging confirmed appropriate alignment, graft positioning, and compression across the scaphoid-trapezial joint.
- Closure: The wound was thoroughly irrigated, and hemostasis was achieved. The joint capsule was closed with interrupted 2-0 FiberWire® in a buried fashion. Subcutaneous tissue was closed with 4-0 Monocryl, and the skin was closed with 4-0 Monocryl in a subcuticular fashion.
A total of 8 cc of Exparel® (bupivacaine liposome injectable) was infiltrated into the superficial and deep tissue layers for postoperative analgesia. - Dressing and Immobilization: A sterile dressing was applied. The patient’s wrist and thumb were immobilized in a well-padded thumb spica cast.
Post-Operative Protocol
- Short arm thumb spica cast for 6 weeks.
Patient Follow-up:
Bone healing across the fusion site was seen as early as 6 weeks from surgery. At the 2-month follow-up, there was clear bone bridging across the fusion site. On her 5-month post-operative visit, her scaphoid-trapezial fusion was fully consolidated at 100%.

AP [A] & [B], Oblique [C] and Lateral [D]
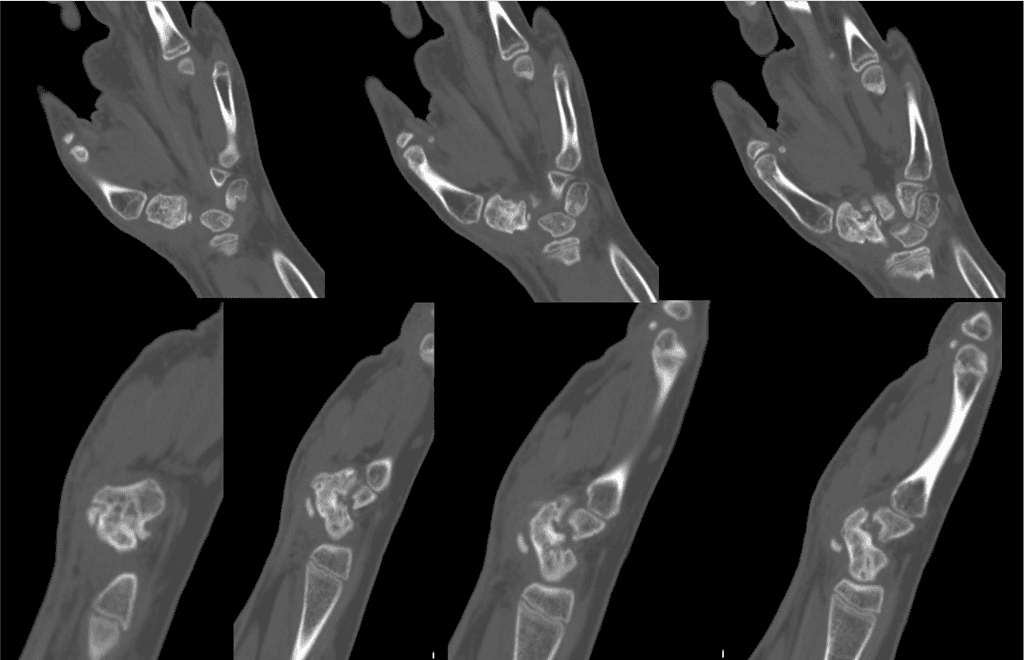
Coronal [top] and Sagittal [bottom]
Summary
I chose OSSIOfiber® for this complex pediatric revision carpal coalition fusion because it provides both solid mechanical stability and biointegrative bone healing, thus avoiding hardware removal which is a huge advantage in a growing child. Hardware removal is one of the most common complications we deal with in pediatric orthopedics, often meaning another surgery with its risks and recovery. Furthermore, the OSSIOfiber® technology offers a unique advantage also in debilitated or high-risk patients where every additional procedure presents the risk of general surgical complications as well as impaired healing.
References
1. Defazio, Michael V et al. “Carpal coalition: A review of current knowledge and report of a single institution’s experience with asymptomatic intercarpal fusion.” Hand (New York, N.Y.) vol. 8,2 (2013): 157-63. doi:10.1007/s11552-013-9498-5
2. Gottschalk, Michael B et al. “Carpal Coalitions and Metacarpal Synostoses: A Review.” Hand (New York, N.Y.) vol. 11,3 (2016): 271-277. doi:10.1177/1558944715614860
3. Hey, Hwee Weng Dennis et al. “Unilateral isolated coalition of the scaphoid and trapezium: a rare incidental finding.” The Journal of hand surgery vol. 38,1 (2013): 207-8. doi:10.1016/j.jhsa.2012.11.004
4. Olmedo, Estefanía M et al. “Radiographic Evolution of Scaphotrapezium Coalition Trough Carpal Ossificaction.” Revista Iberoamericana de Cirugía de la Mano Vol. 51 No. 2/2023 © doi:10.1055/s-00431777112.
5. Christophe L Mathoulin, Max Haerle, Technique: vascularized bone grafts from the volar distal radius to treat scaphoid nonunion, Journal of the American Society for Surgery of the Hand, Volume 4, Issue 1,2004,Pages 4-10, ISSN 1531-0914,
https://doi.org/10.1016/j.jassh.2003.12.004.
