Author: Brian Dix, DPM, FACFAS, Avera Orthopedics, Sioux Falls, SD. Dr. Dix was trained at the prestigious Western Pennsylvania Hospital in Pittsburgh, PA. Board certified by the American Board of Podiatric Surgery, in Foot Surgery, Rearfoot Reconstructive Ankle Surgery.
INTRODUCTION
Hallux valgus is the most common forefoot deformity, with an estimated prevalence of 23% to 35% of population. Choosing the appropriate surgical approach should consider factors such as degree of the deformity and patient clinical symptoms. Lapidus is the preferred procedure for treatment of symptomatic patients with moderate-to-severe deformity. Intercuneiform instability plays an important prognostic role in the Lapidus fixation construct and a potential cause of recurrence. Fleming at el demonstrated that the rate of Intercuneiform instability was 74% in patients treated with Lapidus Arthrodesis. It is believed that stabilization of the Intercuneiform joints as part of Lapidus fusion arthrodesis could be beneficial in controlling the excess motion remaining and conferring additional stability not inherent in this area.1-4
CASE PRESENTATION
This 5-patient case series presents the use of 4.0 OSSIOfiber® Compression Screw (CS) for Intercuneiform instability as part of Lapidus bunionectomy procedure. All patients were female, presented with painful bunion deformity, without significant arthritic changes to the first metatarsal phalangeal (MTP) joint, and all failed conservative treatment. A 1st tarsometatarsal (TMT) joint arthrodesis was discussed and agreed upon by all patients.
WHY OSSIOfiber® IS AN IDEAL CHOICE?
OSSIOfiber® was chosen to provide stable fixation between the medial and middle cuneiforms after a first TMT joint fusion was performed, as there was Intercuneiform instability confirmed intra-operatively. Using OSSIOfiber® CS provides the desired stabilization while avoiding the use of permanent hardware across the Intercuneiform joint.
Preoperative Planning:
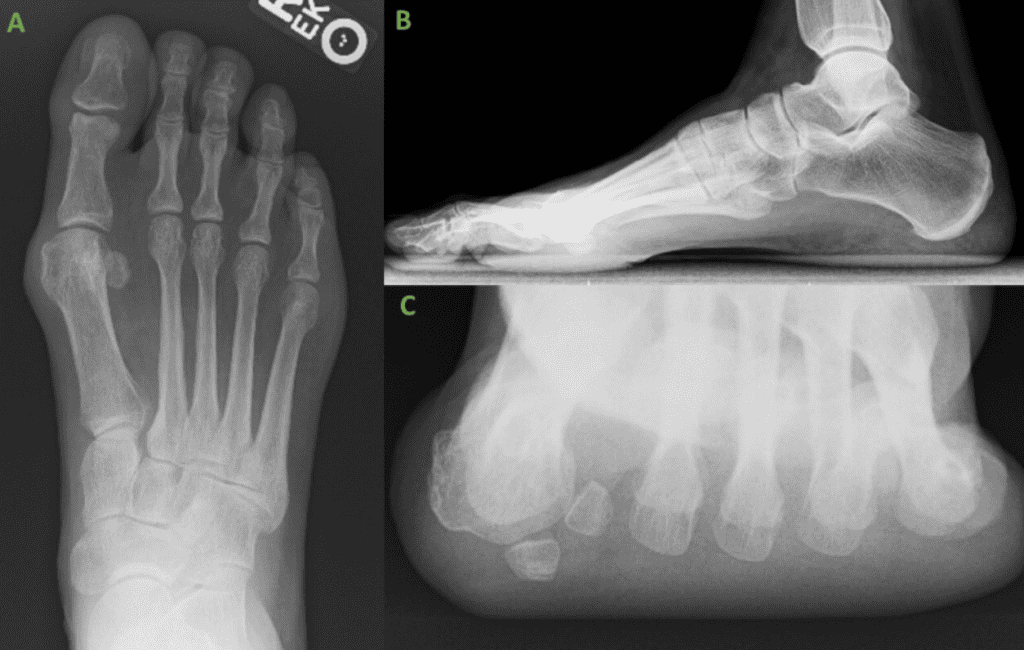
Radiographs of all five patients demonstrated varying degrees of bunion deformity, from moderate to severe, without significant arthritic changes to the 1st TMT joint. All patients had persistent pain and failed conservative treatment. A 1st TMT joint fusion was opted as best treatment option. For one patient an excision of the medial sesamoid was also performed due to painful medial sesamoiditis.
Surgical Procedure:
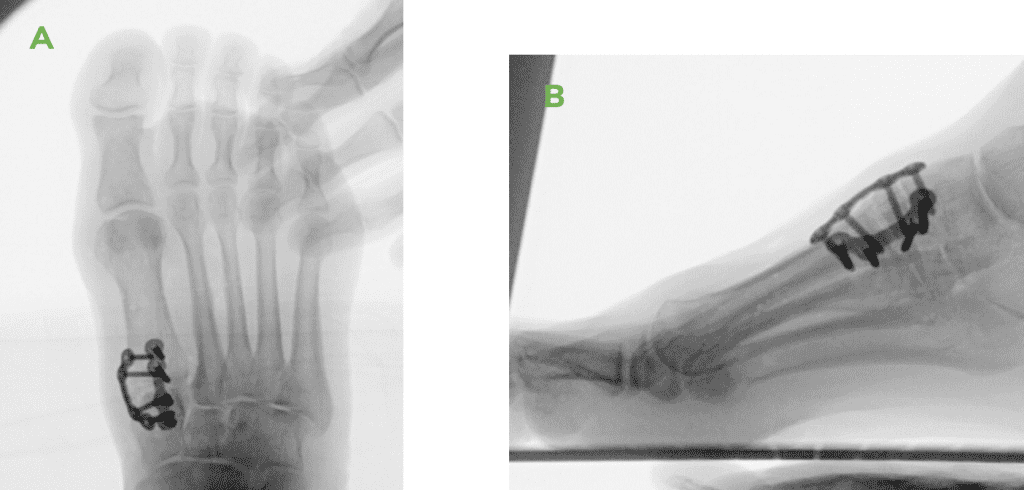
Right 1st TMT joint Fusion with Intercuneiform stabilization.
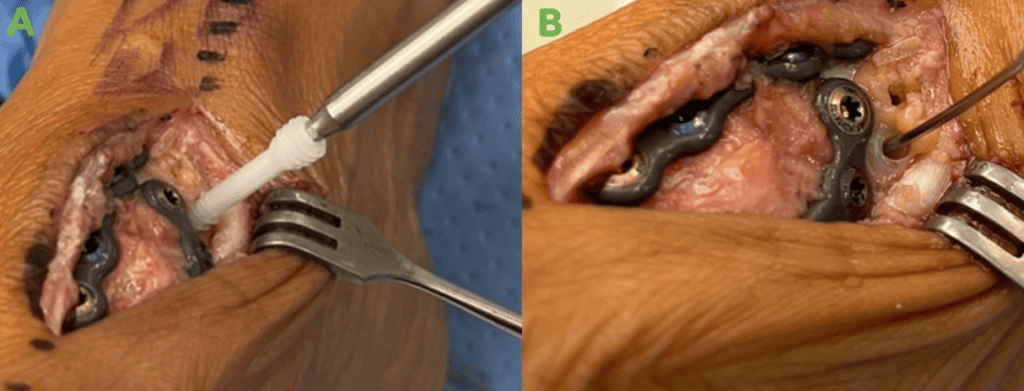
- First TMT joint fixation using Lapiplasty 4 holes plates (Treace Medical Concepts Inc.)
- Intercuneiform fixation using a OSSIOfiber® 4.0x26mm canulated CS
Surgical Technique Steps:
- Dissection / Access: Dissection was performed through the same dorsal medial incision which was utilized for the 1st TMT joint fusion.ssection / Access
– Incision carried down through skin and subcutaneous tissue at the 1st TMT joint.
– The Extensor Hallucis Longus (EHL) tendon identified with the neurovascular bundle and retracted laterally.
– A longitudinal capsulotomy was performed at the 1st TMT joint, exposing the joint surface.
– Joint fusion performed using Lapiplasty 4-hole plates.
Intercuneiform stabilization: - Fixation Site Preparation:
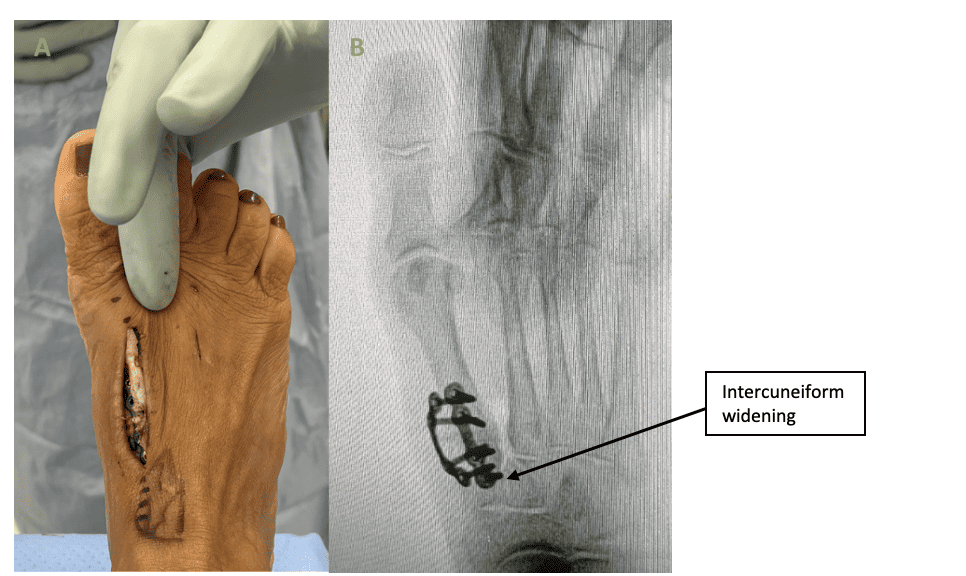
– The medial to middle Intercuneiform joint was stressed by the surgeon, confirming Intercuneiform instability on intra operative fluoroscopy. - Tunnel preparation:
– A K-wire provided in the OSSIOfiber® 4.0 CS instrument kit, was placed from the medial cuneiform to the second cuneiform and position confirmed on fluoroscopy. The dedicated drill bit for the OSSIOfiber® 4.0 CS was then used to create the pilot hole. Pilot hole was then tapped and countersunk. - Implant insertion:
– An OSSIOfiber® 4.0x26mm headless CS was placed using appropriate technique from the medial cuneiform to the middle cuneiform.
– Following screw insertion, the joint was stressed again to confirm no widening is noted. - Closure:
– Subcutaneous 2.0 Vicryl sutures, followed by 4.0 Vicryl Intracuticular and 4.0 Prolene skin sutures.
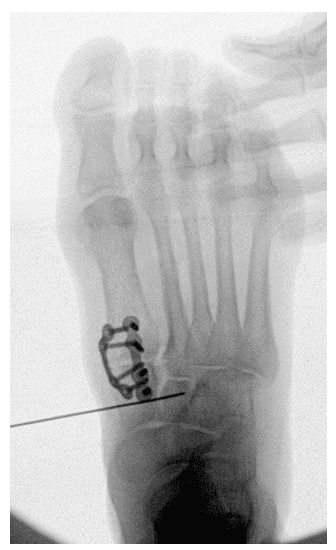
* Technique Pearl: Aim dorsal when placing the guide wire from the medial to intermediate cuneiform, as the intermediate cuneiform base is shallow.

Post-Operative Protocol:
The use of the OSSIOfiber® CS does not alter the standard post-operative instructions for these patients. Non-weight bearing for the first 2-weeks, followed by full weight bearing in a controlled ankle motion walking boot (CAM boot) for additional 4 weeks. At 6-weeks comfort shoe wear.
Patient Follow-Up:
All patients attended their scheduled follow up visits at 1, 2, 4, 6 & 10- weeks with final visit at 4-months. For all patients, healing progressed as expected, full details as follow:
- Week 1: Incision healing nicely with moderate post-op erythema. Patients are non-weight bearing.
- Week 2: Incision has healed nicely after removal of sutures. Mild post op erythema and edema without signs of infection. The great toe is significantly more rectus. Patients can transition to weight bearing in cam boot.
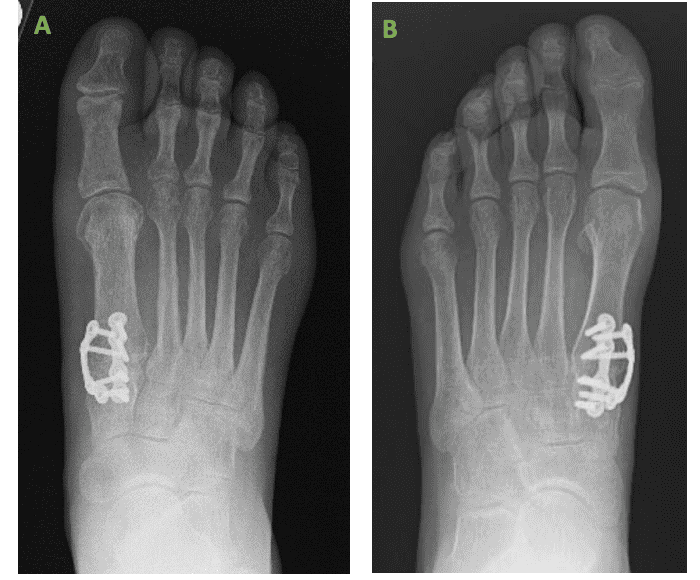
- Week 4-10: Incision has healed nicely. Local erythema resolved. The great toe is significantly more rectus. X-Rays demonstrate reduction of the bunion deformity with a healing first TMT joint fusion and no intercuneiform instability. Patients transitioned to weight bearing in a good supportive tennis shoe and slowly returned to daily activities.
- 4 months: The great toe is significantly more rectus. X-rays samples provided below (Figure 7), show reduction of the bunion deformity with a healed first TMT joint fusion and no Intercuneiform instability. Patients returned to all daily activities in normal shoe wear and most are very pleased with the final results.
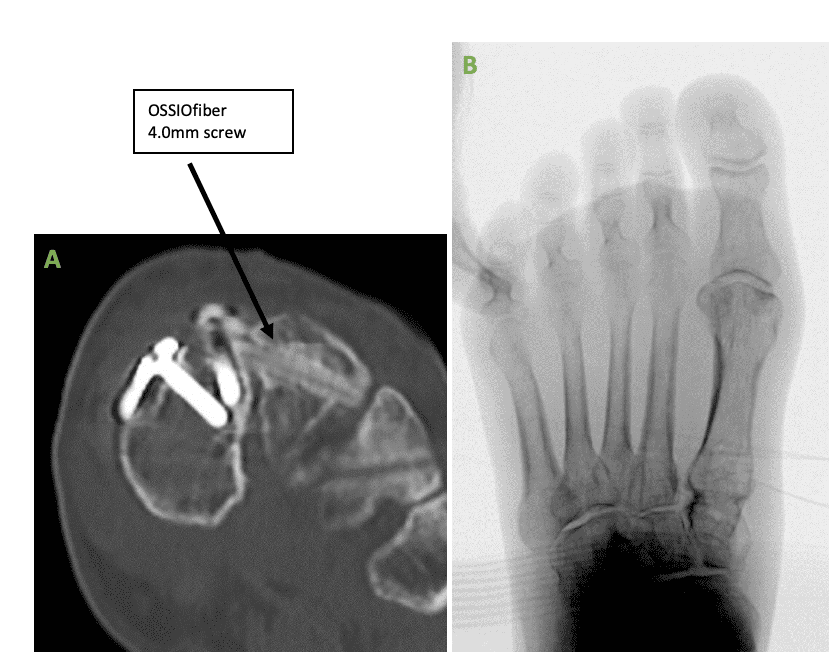
One patient had her follow-up extend beyond the 4 months visit:
- Patient imaging demonstrated full healing at 4-months but the patient had some persistent pain at the surgical site, both dorsal and medial, over the metal plates. At 6-months following the procedure, as the patient continued to demonstrate persistent pain, a decision was made to remove the metal hardware. CT scan was performed showing a healed 1st TMT joint with stable intercuneiform joint and OSSIOfiber® 4.0mm screw. A second surgery was performed, and the dorsal and medial metal plates were removed. Following the removal of the metal hardware, clinical signs have resolved.
Summary:
I chose the OSSIOfiber® 4.0mm cannulated compression screw to address the Intercuneiform instability demonstrated when stressing the Intercuneiform joint following TMT joint plate fusion. I prefer the OSSIOfiber® 4.0mm cannulated screw over a metal screw as I this way I avoid placing permanent hardware across the joint. Furthermore, the screws provide excellent fixation and will not have to be removed in the future as they incorporate within the bone over time.
References
1. The treatment of hallux valgus. Wülker N, Mittag F. Dtsch Arztebl Int. 2012 Dec;109(49):857-67; quiz 868. doi: 10.3238/arztebl.2012.0857.
2. Intraoperative evaluation of medial Intercuneiform instability after Lapidus arthrodesis: Intercuneiform hook test. Fleming JJ, Kwaadu KY, Brinkley JC, Ozuzu Y. J Foot Ankle Surg. 2015;54:464–472.
3. Enhanced Lapidus arthrodesis: crossed screw technique with middle cuneiform fixation further reduces sagittal mobility. Galli MM, McAlister JE, Berlet GC, Hyer CF. J Foot Ankle Surg. 2015;54:437–440
4. Recurrence of Hallux Valgus After Modified Lapidus Procedure With Successful Fusion of the Intermetatarsal and Intercuneiform Joints. Long J, Lauf JA, Whitehead B, Cheney N, Law TD.. Cureus. 2021 Jun 3;13(6):e15418. doi: 10.7759/cureus.15418. PMID: 34249565; PMCID: PMC8254418.
Medical professionals must use their professional judgment for patient selection and appropriate technique.
Results from case studies are not predictive of results in other cases. Results may vary.
Please refer to the product instructions for use for warnings, precautions, indications, contraindications and technique.
Not available for sale outside of the US. Speak to your local sales representative for product availability.
For more information, please visit ossio.io
® OSSIO and OSSIOfiber® are registered trademarks of OSSIO Ltd.
All rights reserved 2022.
DOC-002300 Rev 1.0
