Author: Brian Dix, DPM, FACFAS, Avera Orthopedics, Sioux Falls, SD. Dr. Dix was trained at the prestigious Western Pennsylvania Hospital in Pittsburgh, PA. Board certified by the American Board of Podiatric Surgery, in Foot Surgery, Rearfoot Reconstructive Ankle Surgery.
INTRODUCTION
Hallux valgus is the most common forefoot deformity, with an estimated prevalence of 23% to 35% of population. Choosing the appropriate surgical approach should consider factors such as degree of the deformity and patient clinical symptoms. Lapidus is the preferred procedure for treatment of symptomatic patients with
moderate-to-severe deformity. Intercuneiform instability plays an important prognostic role in intraoperative rate of the Lapidus fixation construct and a potential cause of recurrence. Fleming at el demonstrated that the rate of Intercuneiform instability was 74% in patients treated with Lapidus Arthrodesis. It is believed that
stabilization of the Intercuneiform joints as part of Lapidus fusion arthrodesis could be beneficial in controlling the excess motion remaining and conferring additional stability not inherent in this area.1-4
CASE PRESENTATION
A 62-year-old, 75Kg female patient, presented with a painful right bunion deformity without significant arthritic changes to the first metatarsal phalangeal joint, who failed conservative care. A 1st tarsometatarsal (TMT) joint arthrodesis was discussed and agreed upon.
WHY OSSIOfiber® IS AN IDEAL CHOICE?
OSSIOfiber® was chosen to provide stable fixation between the medial and middle cuneiforms after a 1st TMT joint fusion was performed, as there was Intercuneiform instability confirmed intra-operatively. Using OSSIOfiber® Compression Screw provides the desired stabilization while avoiding the use of permanent hardware across the Intercuneiform joint.
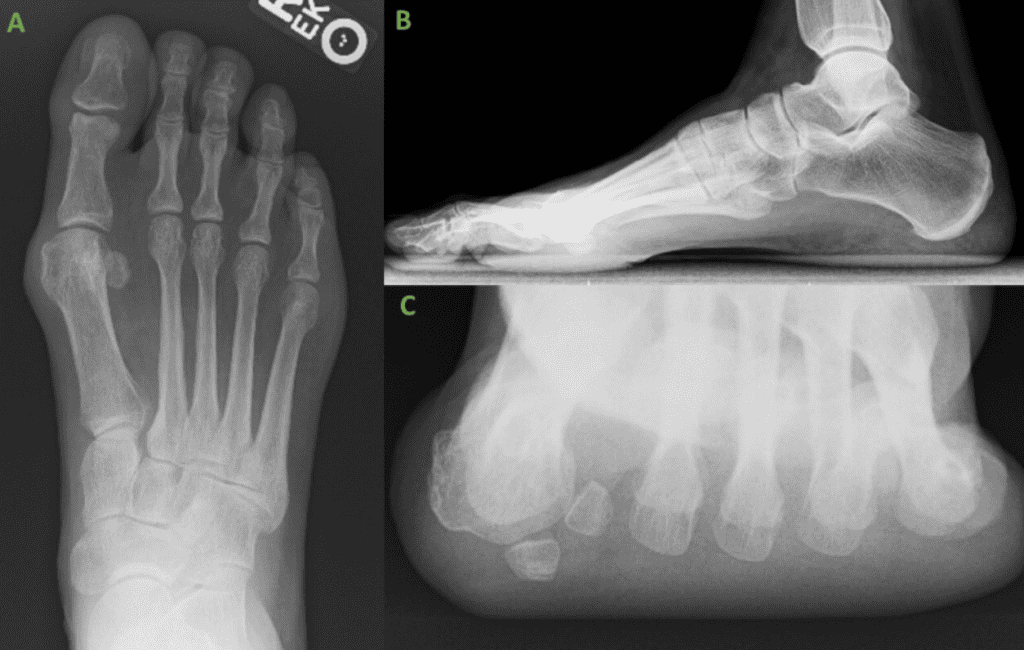
Preoperative Planning:
Radiographs of the right foot demonstrated a moderate to severe bunion deformity without significant arthritic changes to the 1st TMT joint. The patient failed conservative management and had consistent pain on daily basis. Thus, surgery was discussed, and a 1st TMT joint fusion was opted as best treatment option.
Surgical Procedure:
Right 1st TMT joint Fusion with Intercuneiform stabilization.
- First TMT joint fixation using Lapiplasty 4 holes plates (Treace Medical Concepts Inc.)
- Intercuneiform fixation using a OSSIOfiber® 4.0x26mm canulated CS
Surgical Technique Steps:
- Dissection / Access: Dissection was performed through the same dorsal medial incision which was utilized for the 1st TMT joint fusion.ssection / Access
– Incision carried down through skin and subcutaneous tissue at the 1st TMT joint.
– The Extensor Hallucis Longus (EHL) tendon identified with the neurovascular bundle and retracted laterally.
– A longitudinal capsulotomy was performed at the 1st TMT joint, exposing the joint surface.
– Joint fusion performed using Lapiplasty 4-hole plates. - Intercuneiform stabilization:
– Fixation Site Preparation:
The medial to middle Intercuneiform joint was stressed by the surgeon, confirming Intercuneiform instability on intra operative fluoroscopy. - Tunnel preparation:
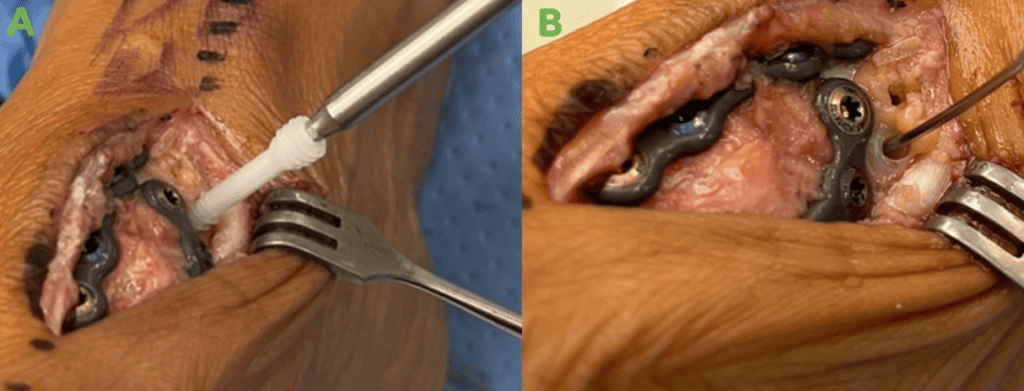
A K-wire provided in the OSSIO®Compression Screw instrument pack, for 4.0mm screws, was placed from the medial cuneiform to the second cuneiform and position confirmed on fluoroscopy. The dedicated drill bit for the OSSIOfiber® 4.0 CS was then used to create the pilot hole. Pilot hole was then tapped and countersunk. - Implant insertion:
– An OSSIOfiber® 4.0x26mm Compression Screw was placed using appropriate technique from the medial cuneiform to the middle cuneiform.
– Following screw insertion, the joint was stressed again to confirm no widening is noted. - Closure:
– Subcutaneous 2.0 Vicryl sutures, followed by 4.0 Vicryl Intracuticular and 4.0 Prolene skin sutures.
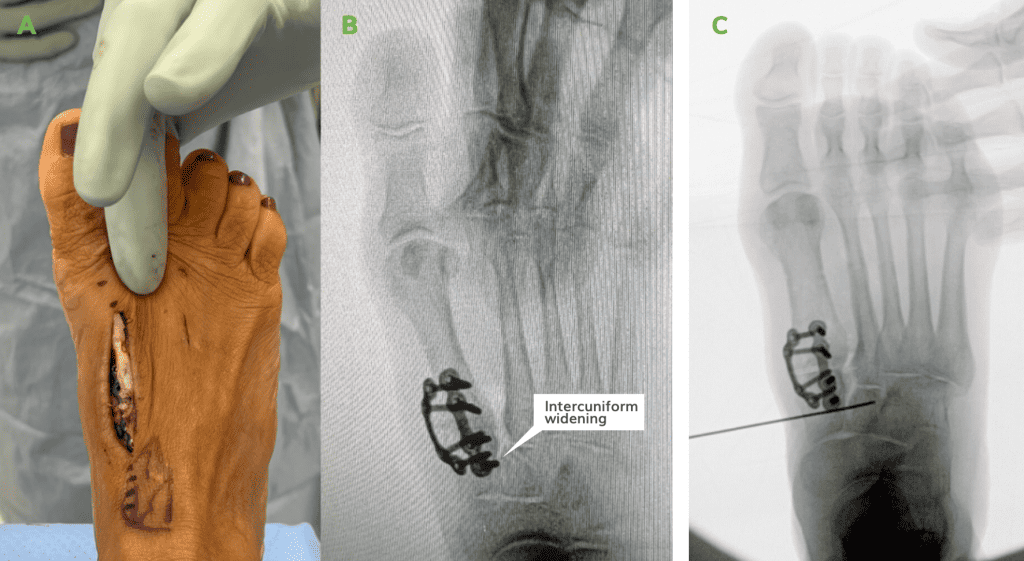
Figure 3: AP view of the placement of the guide wire to the lateral border of the middle cuneiform for the insertion of a cannulated OSSIOfiber® 4.0mm CS.
*Pearl: Aim dorsal when placing the guide wire from the medial to intermediate cuneiform, as the intermediate cuneiform base is shallow.

* Technique Pearl: Aim dorsal when placing the guide wire from the medial to intermediate cuneiform, as the intermediate cuneiform base is shallow.
Post-Operative Protocol:
The use of the OSSIOfiber® CS does not alter the standard post-operative instructions for these patients. Non-weight bearing for the first 2-weeks, followed by full weight bearing in a controlled ankle motion walking boot (CAM boot) for additional 4 weeks. At 6-weeks comfort shoe wear.
Patient Follow-Up at 25 Weeks:
The patient attended all scheduled visits, at 1, 2, 4, 6 & 10- weeks with final visit at 4-months. Healing progressed as expected, full details as follow:
- Week 1: Incision healing nicely with moderate post-op erythema. Patient non-weight bearing.
- Week 2: Incision has healed nicely after removal of sutures. Mild post op erythema and edema expected at this stage of healing. Right great toe is significantly more rectus. Patient can transition to weight bearing in cam boot.
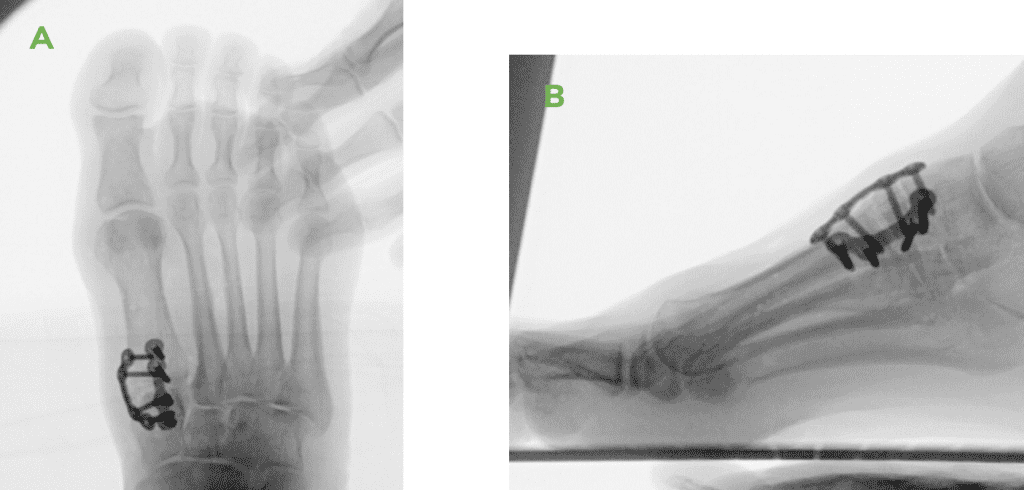
- Week 4-10: Incision has healed nicely. Local erythema resolved. Right great toe is significantly more rectus. X-Rays demonstrate reduction of the bunion deformity with a healing 1st TMT joint and no Intercuneiform instability. Patient transitioned to weight bearing in a good supportive tennis shoe and slowly returned to daily activities.
- 4 months: Right great toe is significantly more rectus. X-rays, provided below (Figure 7), show reduction of the bunion deformity with fused TMT joint and no Intercuneiform instability. Patient has returned to all daily activities in her normal shoe wear and is very pleased with the final results.

Summary:
I chose the OSSIOfiber® 4.0mm Compression Screw to address the Intercuneiform instability demonstrated when stressing the Intercuneiform joint following 1st TMT joint plate fusion. I prefer the OSSIOfiber® 4.0mm screw over a metal screw as OSSIOfiber® screws provide excellent fixation and will not have to be removed in the future as it will incorporate within the bone over time.
References
1. The treatment of hallux valgus. Wülker N, Mittag F. Dtsch Arztebl Int. 2012 Dec;109(49):857-67; quiz 868. doi: 10.3238/arztebl.2012.0857.
2. Intraoperative evaluation of medial Intercuneiform instability after Lapidus arthrodesis: Intercuneiform hook test. Fleming JJ, Kwaadu KY, Brinkley JC, Ozuzu Y. J Foot Ankle Surg. 2015;54:464–472.
3. Enhanced Lapidus arthrodesis: crossed screw technique with middle cuneiform fixation further reduces sagittal mobility. Galli MM, McAlister JE, Berlet GC, Hyer CF. J Foot Ankle Surg. 2015;54:437–440
4. Recurrence of Hallux Valgus After Modified Lapidus Procedure With Successful Fusion of the Intermetatarsal and Intercuneiform Joints. Long J, Lauf JA, Whitehead B, Cheney N, Law TD.. Cureus. 2021 Jun 3;13(6):e15418. doi: 10.7759/cureus.15418. PMID: 34249565; PMCID: PMC8254418.
Medical professionals must use their professional judgment for patient selection and appropriate technique.
Results from case studies are not predictive of results in other cases. Results may vary.
Please refer to the product instructions for use for warnings, precautions, indications, contraindications and technique.
Not available for sale outside of the US. Speak to your local sales representative for product availability.
For more information, please visit ossio.io
® OSSIO and OSSIOfiber® are registered trademarks of OSSIO Ltd.
All rights reserved 2022.
DOC-002300 Rev 1.0
